Hypermobility
Hypermobility is a common condition that affects 1 in 20 people. Research has shown that 10-25% of children have hypermobility. The symptoms will usually be most obvious between the ages of 13 and 19 years old with the majority of patients presenting at age 15. Girls have been found to be more affected than boys.

HYPERMOBILITY CLASSIFICATION
Ehlers-Danlos Syndromes (EDS) are a group of connective tissue disorders that can be inherited and are caused by a gene mutation. They are characterised by joint/ skin hypermobility and tissue fragility.
Hypermobility Spectrum Disorders (HSD) are a group of conditions involving joint hypermobility which are diagnosed after excluding EDS types and other conditions.
HOW A PATIENT CAN PRESENT
Hypermobility can present in a variety of ways which are commonly age dependant. Children will often present with lower limb muscle weakness and have poor proprioception. While adults who present with hypermobility often will report a history of dislocations, subluxations, fatigue, chronic headaches and back pain.
Hypermobility does not solely affect the musculoskeletal system. It is well known that neural, vascular and digestive structures can also be affected. In more complex presentations, HSD and EDS are also associated with dizziness, anxiety and sleep disturbances.
DIAGNOSIS
Typically patients will wait years or decades for a diagnosis of EDS, if they get one at all. Common misdiagnoses include fibromyalgia, chronic fatigue syndrome and irritable bowel syndrome, when the patient has associated digestive problems.
In 2017, the American Journal of Medical Genetics published new terminology and internationally agreed upon an EDS classification.
Hypermobility is now classified using the idea of a spectrum. At one end, is simply the physical trait of hypermobility without any disease. At the other end of the spectrum is the thirteen subtypes of EDS. In between falls a range of hypermobility-related conditions called hypermobility spectrum disorders (HSD).
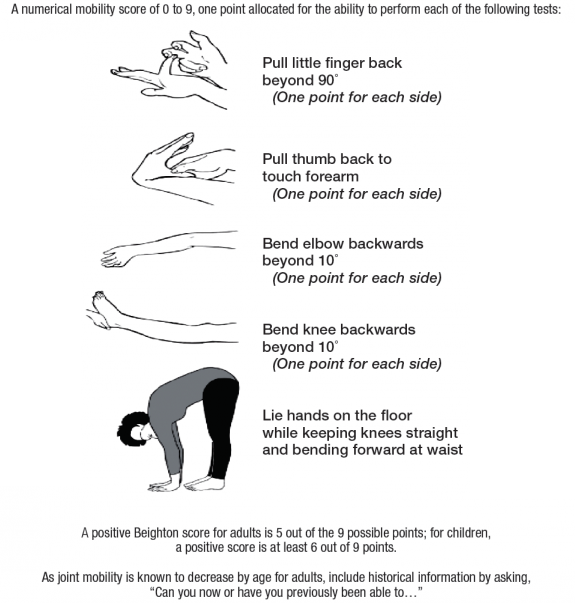
The Beighton Score is a simple system that quantifies hypermobility. If diagnosed, a referral can be made to a Rheumatologist or a Clinical Geneticist.
HYPERMOBILITY AND INJURY
Hypermobility is a risk factor for musculoskeletal problems, predominantly due to the passive structures being more fragile and therefore prone to small repetitive injuries. Being hypermobile will increase the risk of dislocation and failure of ligaments.
Surprisingly, hypermobile individuals often present with a feeling of joint stiffness. The reason is because the body will try to find a way to create stability surrounding a vulnerable joint. The large, superficial muscles will increase their activity in support of the lax joint, therefore restricting motion. Unfortunately this often results in pain and injury. This excessive gripping makes movement and prolonged positions fatiguing.
Proprioception is also found to be reduced in people with hypermobility. This is the awareness of ones body position and movement in space, without visual input.
EARLY INTERVENTION
Early detection and understanding the symptoms are key to addressing Hypermobility. For children, screening is essential within their specific sports. Once the hypermobile individuals are identified, they can be given a specific prehabilitation program to prepare them for potential high risk environments. If undetected or not diagnosed early enough, it is possible that a severe injury could lead to irreversible joint damage and lifelong implications.
PHYSIOTHERAPY TREATMENT
Treatment would begin with patient education and teaching coping strategies. Establishing objective baseline measurements and initial level of activity are essential in creating achievable short and long term goals. A home exercise program would be adjusted for both good and bad days to improve cardiovascular fitness, strength, joint stability, proprioception, balance and mobility. Manual therapy can also be a useful tool in alleviating muscle spasm
Taping techniques are useful for posture correction, joint protection, and/or movement facilitation. A Physiotherapist should continually monitor the progress of the patient and upgrade exercises as required. It is inevitable that hypermobile patients will have set backs or flare ups throughout their lives and it is important to have a health professional they can reach out to for support and oversee their management.
Want to find out more, speak to one of our team members or book in for an appointment today!
References
– https://www.ehlers-danlos.org/
– https://www.ehlers-danlos.com/
– Hypermobile Ehlers-Danlos syndrome: Clinical description and natural history (https://pubmed.ncbi.nlm.nih.gov/28145611/)


Sorry, comments are closed for this post.