Concussion and Physiotherapy
Definition: ” A traumatic brain injury (TBI) induced by biomechanical forces” (McCrory et al., 2017)

EVIDENCE FOR PHYSIOTHERAPY REHABILITATION FOR CONCUSSION
Systematic Review – Schneider et.al. 2017:
“A brief period (24-48 hrs) of cognitive rest is appropriate for most patients. Following this, patients should be encouraged to gradually increase activity. The exact amount and duration of rest are not yet well defined and require further investigation. The data support interventions including cervical and vestibular rehabilitation and multifaceted collaborative care. Closely monitored sub-symptom threshold, submaximal exercise may be of benefit.”
In 2010, researchers first showed that specialised exercise regimens can relieve prolonged concussion symptoms.

WHAT IS THE ROLE OF PHYSIOTHERAPY
- On field assessment (side-line)- identification and emergency response
- Initial assessment in the clinic:
- Cervical spine range of motion
- Upper and lower limb neurological testing
- Gait and balance
- Mental status
- Sleep pattern/disturbances
- Occular/vestibular function
TREATMENT AND REHABILITATION
Physiotherapy for concussion is patient specific and includes the following:
- Education and reassurance
- Concussion explanation
- Moderate rest and early activation- encourage light exercise. Insufficient evidence for complete rest
- Signs and symptoms to look out for
- Importance of rehabilitation
- Potential psychological effects of concussion (anxiety, withdrawal)
- Manual therapy
- Massage
- Joint mobilisation
- Rehabilitation and guidance
- Research supports early psychological, vestibular, cervical interventions as well as closely monitored active rehabilitation programs
- Individualised rehabilitation
- Cervical spine ROM exercises
- Breathing exercises
- Balance training
- Exercise programs that are tailored around the patients social sporting activities
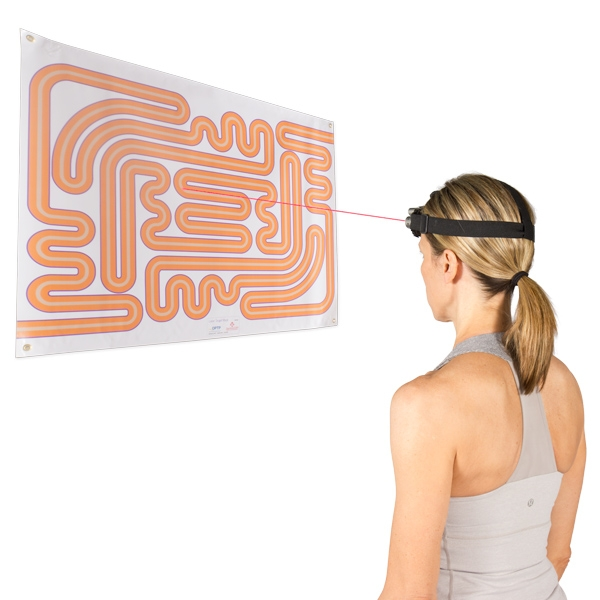
- Vestibular therapy: BPPV, Nystagmus
- Vision therapy: Convergence/divergence
- Nutritional advice and education
- Referral to multi-disciplinary specialists as required
Outcome measures used for concussion to help diagnose and assess improvements in physical and cognitive function
- Maddock’s questions
- SCAT 5
- Cogsport
- HeadSmart
RETURN TO LEARN, WORK AND PLAY
- Full recovery is classified as “a resolution of post cuncussion symptoms and return to normal balance and cognitive function”
- Limited evidence to support medication use
Want to learn more about concussion management contact our team today or book in an appointment online.
References:
- Leddy, J.L., Sandhu, H., Sodhi, V., Baker, J.G., & Willer, B. (2012). Rehabilitation of concussion and post-concussion syndrome. Sports Health, 2(4), 147-154. doi:10.1177/1941738111433637
- McCrory, P., et al. (2017). Consensus statement on concussion in sport: the 5th international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine. 0:1–10. doi:10.1136/bjsports-2017-097699
- Schneider, K.J., Leddy, J.J., Guskiewicz, K.M., Seifert, T., McCrea, M., Silverberg, N.D., Feddermann-Demont, N., Iverson, G., Hayden, A., & Makdissi, M. (2017). Rest & treatment/rehabilitation

