Meniscal Tears: A modern approach

BACKGROUND:
Meniscal tears are one of the most frequently encountered knee injuries across peoples lifespan from sports injuries to degenerative tears. A common presentation could be an inability to straighten the knee fully, severe pain, swelling, and possibly catching, clicking, difficulty on deep knee bending and locking of the knee in partial flexion .
We have seen a dramatic shift in management of these injuries from the traditional “if it is torn, take it out” to a “save the Meniscus” approach (1). The importance of the preservation of the meniscus has been recognised in reducing knee pain and disability later in life.
STRUCTURE:
The two menisci, medial and lateral, and fibrocartilaginous soft tissue structures in the tibiofemoral joint that are totally vascularised at birth, and by adulthood are limited to 10-30% vascularisation of the peripheral zone only. What does that mean? This change in vascularisation reduces the rate of natural healing occurring in the menisci. Its vital functions are load bearing, joint stability, joint congruency, decreasing joint contact area, protecting articular cartilage, shock absorption and joint proprioception i.e. the ability to judge where your joint is in space ( bent or straight etc.) (1).
MANAGEMENT
Operative
Arthroscopic knee surgery for degenerative knee disease, including meniscal tears, is the most common orthopaedic procedure in countries with available data. These operative techniques include: arthroscopic partial menisectomy; meniscal repair; meniscal reconstruction.
2016 Meniscus Consensus Project summary:
| Surgery should not be considered the first line treatment choice |
| Surgery should only be proposed after a proper standardised imaging protocol |
| Proposed >3 months of persistent pain / mechanical symptoms or earlier if significant symptoms. |
| Should not be performed with advanced OA on XRAY |
Non-operative management:
Hello Physio! Non- operative management is useful in the initial treatment of acute knee trauma and as a first-line treatment method in degenerative meniscal tears. Please note that bracing is usually not required, unless combined with an MCL or LCL injury, or if there is a mechanical ROM restriction.
ACUTE INJURY– POLICE Protocol – Protect, Optimally Load, Ice, Compression, Elevation (Instead of RICE protocol
DEGENERATIVE MENISCAL PATHOLOGY– anti-inflammatory and analgesic medications, +- intra-articular injections
EXERCISE – Both categories of meniscal tears then benefit from a structured exercise based rehabilitation program, including quadriceps activation / strengthening, neuromuscular control and proprioception, lower limb kinetic chain strengthening and gait re-training.

The recommendation is 3-6 months of combined conservative management techniques unless mechanical symptoms dominate the picture.
So why the shift from operative to non-operative care?
Well, traditionally partial menisectomy surgery demonstrated highly successful short term results. However it was found within long term studies a high rate of progression to osteoarthritis post operative. We also know that not all meniscal tears are symptomatic. Some research indicates 60% of people over the age of 50 have meniscal tears and no pain.
There is now current high level of evidence and research that into long term clinical trials and what they have shown is an absence of long term clinical benefit between menisectomy and non-operative or sham treatments.
What can health professionals do to help you?
The consensus from the Orthopaedic community is that they should exhaust non-operative management before contemplating surgery to protect the joint in the long term from the early development of osteoarthritis. Even at this point, it is preferable to attempt repair or reconstruction over resection or menisectomy.
Health professionals are able to provide better patient care when they can properly educate patients on the nature of their pain, and how it relates to their meniscal tears.
Let’s work together!
Collectively, GPs and Physiotherapists can work together to assess a client and determine who needs early referral to an Orthopaedic Surgeon for review, or who can at least commence non-operative management before making that referral. Together, this can assist in protecting the function of the knee, restoring early ROM and function of the knee and reduce pain scores and secondary biomechanical pains.
Have a chat with one of our team members today!
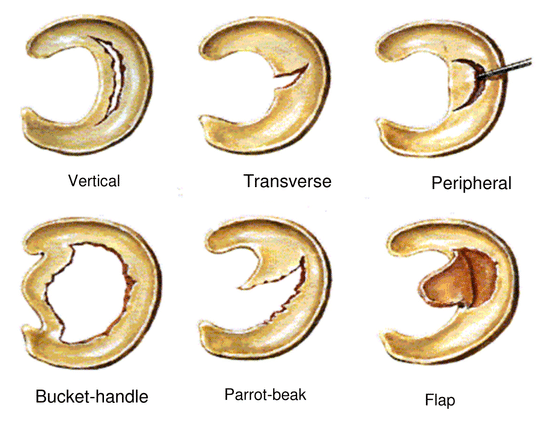
References: (1) Modern treatment of Mensical Tears, Doral et al (2018) – EFORT Open Review, May 2018 (2) Arthroscopic surgery of degenerative knee OA and mensical tears (Siemieniuk et al), BJSM 2018 (3) Effect of early surgery vs physical therapy on knee function among patients with non-obstructive meniscal tear ( Physio Network Peer Review, T Hargrove) Image Reference: https://totalphysiocare.com.au/meniscus-tear/ https://kneeandshoulderclinic.com.au/knees/surgical-conditions/meniscal-tears/


Sorry, comments are closed for this post.