
Lateral Hip Pain Part 2
PART 2 GLUTEAL TENDINOPATHY
CALM AND SUPPORT THE HIP
As you read in our previous blog, diagnosis of Gluteal Tendinopathies (GT) can be quite complicated. It is quite common in physio to see patients who present with lateral (side) hip pain that have been unresponsive to treatment for their primary diagnosis, such as greater trochanteric bursitis or lumbar referred pain. Patients that continue to experience pain may in fact be experiencing GT and will respond better to specific rehabilitation.
What do physios do next?
TREATMENT
Accurate diagnosis through history taking and physical clinical tests is essential in the treatment of any tendinopathy. Your physiotherapist will then decide if whether you require manual therapy techniques to assist with reducing your pain. Treatment is directed at reducing the compression forces around the hip.
These may include
- soft tissue massage
- dry needling
- radial shockwave therapy
(for those that don’t know what dry needling or shockwave are… perhaps a topic for another day)
EDUCATION
Physios EDUCATE on pathology, anatomy and biomechanics, teach you how to sit, stand and walk. All with desired outcome of decreasing the compression forces around your hip. If you don’t understand what it is and what’s going on and why it occurred you will continue to aggravate your symptoms.
Physios need to teach good postural habits
- not standing in a way that your lower limb is crossing mid-line (hip adduction)
- reduce crossing legs in sitting and knees together postures. We may even need to get your families involved to remind you “you’re crossing your legs again!”
- advising not to sit too spread legged either, as this also places compression on the hips
- low seats are a problem- we might suggest wedge cushions to open up your hips more, recliner chairs in the evenings- but no crossing of legs!
- night time- lying on an eggshell mattress overlay helps with decompression
- a big pillow in between your knees when you lie on your unaffected side to keep the hips in a resting neutral position instead of knees together
IS STRETCHING SAFE ALL THE TIME?
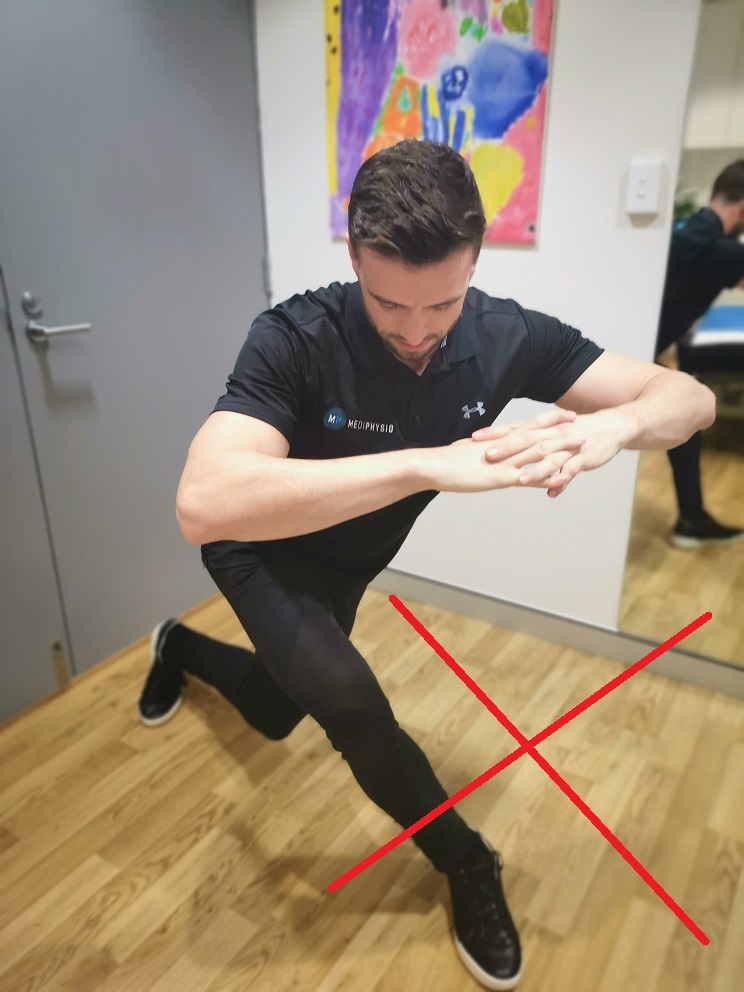

- NO ITB stretches, or flexion adduction stretches! Don’t want further compression against an already sore structure -used to be the approach to stretch, but not anymore
- does the hip flexor feel tight because it’s weak?
- massage is better!
- trigger point releases with a tennis ball or massage ball (not too hard and not on the side of the hip) at home are better than stretches
EXERCISE
Physios prescribe specific rehabilitation! Tailored for each individual and their everyday needs in sporting, workplace and their everyday life.
You should then be prescribed a multi-stage exercise program
1) Isometric exercises, which significantly assists with reducing tendon pain in the early stages
2) Strength training (higher progressive loading) of specific muscles groups
3) Functional strength, challenging balance and progressing to more single legged strength, endurance and proprioception

4) Sport specific training such as diagonal running, plyometrics, ball drills etc
Throw in some biomechanical analysis in there too (probably done early, during and at the end)
– gait retraining is a must
– footwear & potential orthotics assessment if required
Exercise recommendations from physios:

- recruiting your abductors in the right way with palpation (touching of the muscles bellies) which your physio should show you how to do
- single legged static contractions, such as standing and holding against the wall
- NO CLAMS, NO LEG LIFTS
- avoid open chain (where your foot is not in contact with anything) initially, as this recruits too much of your superficial muscle system and not your deep stabilisers around your hip
- closed chain (foot in contact with something, ground, foot plate) is better e.g. bridging (don’t lift too high)- single leg bridge- one foot gradually creeps forward, transverse abdominus and pelvic floor retraining, glut max contractions, mini squats, STS practice
- hand support to assist balance in the early stages is important, then challenge balance later on functionally and sports specifically
- don’t progress too quickly

Bridging with a swiss ball can increase the balancing difficulty as it is an uneven surface
Factors to consider for lack of improvements in symptoms:
- still doing across body stretching, NO DEAL! Stop immediately!
- not adequate enough activity modification for long term factors- go back and revisit physio and check.
- how are you sitting, standing, walking?
- general exercise load progressions throughout week. Are you over doing it on one day and not resting enough the next day?
- rapidly progressing into single leg tasks before having adequate control
If you, or someone you know is complaining of lateral (side) hip pain. They may have a Gluteal Tendinopathy (GT) and may need a review and guidance from a physiotherapist. Contact our team today!
In this blog are just some guidelines and information that we find useful and interesting. We ALWAYS recommend patients have a thorough physical assessment with a physiotherapist and have an exercise and management plan specifically tailored to them. THIS IS SO IMPORTANT!



