LUMBAR DISC INJURIES AND PHYSIO
What are lumbar disc injuries?
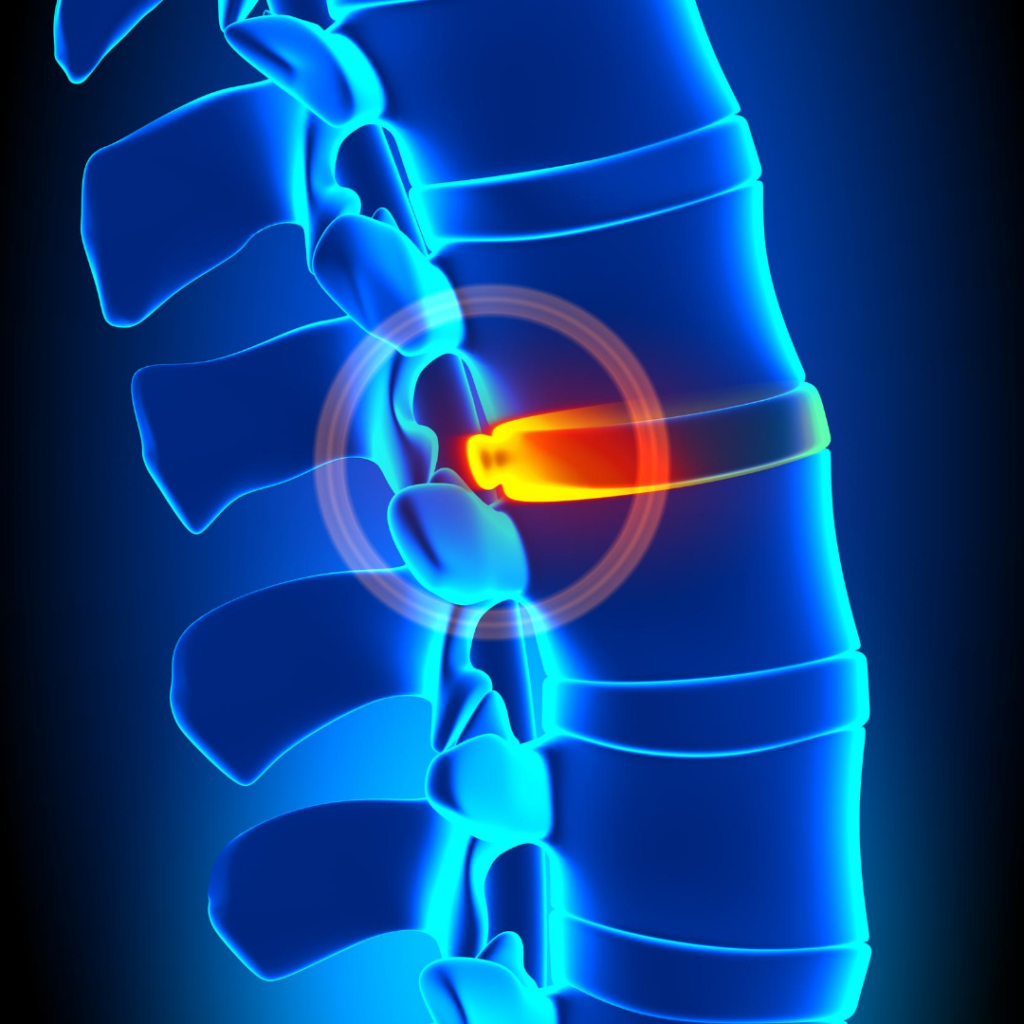
The area between the lumbar vertebral bodies and sacral vertebral bodies is a transition zone. It is at increased risk of injury due to the change in biomechanics that occurs between these regions. Separating each vertebral body of the spine are pads of fibrocartilage based structures that provide support, flexibility, and minor load sharing, known as the intervertebral discs. An injury to the normal architecture of the annulus fibrosus of the disc can lead to degeneration or a protrusion of the inner nucleus pulposus. This can possibly apply pressure to the spinal cord or nerve root and can result in pain and weakness (Gregory et al, 2017).
More than 90% of herniated discs occur at the L4-L5 or the L5-S1 disc space. If the disc injury progresses to the point of neurological compromise or limitations with activities of daily living, then surgical intervention may be required to decompress and stabilise the affected segments. In the absence of motor deficits, a nonoperative course of analgesia, activity modification and injections should be tried for several months.
Interesting

Interestingly, while a common belief is that repetitive forward flexion actions correlate with disc injury, no studies correlate to a dose-response relationship between physical loading and disc injury. It is now thought that the literature on intervertebral disc disease once associated with these heavy physical loading in occupations, may be confounded by correlations with a lower socioeconomic status or lifestyle factors (Gregory et al, 2017).
EDUCATION AND PROGNOSIS
We often hear the terminology of discs slipping. The interesting thing about the vertebral end plate is that there is both a bony and cartilaginous end-plate that create an exceptionally strong connection to the annulus of the disc, making it impossible for the disc to slip (Chiu et al,2018).
The first step in the management of disc related back pain at Mediphysio is Education. Education using the correct terminology and positive reinforcement surrounding the positive natural history for disc injuries (Chiu et al, 2018).
We use the evidence from Chia et al who performed a systematic review examining the evidence of the intervertebral disc to heal. They found that the rate of spontaneous regression was 96% for sequestration, 70% for disc extrusion, 41% for disc protrusion and 13% for disc bulging. This means that the larger the disc injury, the greater likelihood that it will heal. We find that this information surrounding prognosis can have a significant calming and analgesic effect on the patient and provides confidence to move and return to normal activities.
MANAGEMENT OF DISC INJURIES
- Treatment Triage: The physio’s main aim initially is to decide if this patient requires imaging and orthopaedic referral depending on the degree of neurological involvement.
- If there is no nerve root involvement, advice and guidance in collaboration with the GP is required to discuss optimal medication management or further imaging.
- Treatment can be matched to three sub-classifications of disc related back pain.
- Disc related mechanical back pain
- Disc herniation with nerve mechonsensitivity
- Disc herniation with radiculopathy
TREATMENT

- Acute 1-5 days: Pain can be quite severe. Generally patients do not respond well to manual therapy at this stage. However, some neural desensitising techniques in side lying can work well for those with nerve root involvement. We focus on education, reassurance, pain management and encourage movement. Trying to find the balance between letting a patient’s pain settle and encouraging movement is important.
- We generally encourage them to find a position of ease, walk in small doses during the day and avoid resting for long periods of time.
- Normalising pain is important and its to be expected.
- Heat packs and lumbar supports may be appropriate in this acute stage.
- Sub-acute: Massage, joint mobilisations and lumbar directional preference can guide exercise specific to the patient.
- Conditioning: Lumbo-pelvic strengthening exercises and cardiovascular activities should be encouraged when the pain has settled.
- Resume normal activities; It is important to encourage the patient to return to their normal activities.
- It’s important that the patients returns with confidence, minimal guarding with movement and very little fear (Schoenfield et al, 2018)

PHYSIOTHERAPY TREATMENT SUMMARY (Lumbar disc injuries)
The most recent guidelines for conservative management of disc related pain consist of:
ACUTE:
- Education
- education, reassurance, pain management and encouraging movement
- Lumbar supports/braces
- Heat packs
- Nerve gliding (neuro-dynamic) exercises for those with nerve root involvement
- neural desensitising techniques in side lying
Activity modification, moving small amounts frequently and avoiding long periods of rest
SUB-ACUTE:
- Massage, joint mobilisations
- Lumbar directional preference exercise
- Lumbar Mobility exercises
- Lumbo-pelvic strengthening
- Return to cardiovascular exercise
Disc related back pain treatment should be specific for each individual case as not all patients will require all treatments. Scientific evidence will not be able to guide the tailoring of interventions. Come and see one of the Mediphysio team physios today!
References: Gregory DS, Seto CK, Wortley GC, Shugart CM. Acute lumbar disk pain: navigating evaluation and treatment choices. Am Fam Physician. 2008;78:835–842 -The probability of spontaneous regression of lumbar herniated disc: a systematic review (Chiu,2018) Clinical rehabilitation-Treatment of lumbar disc herniation: Evidence-based practice (Schoenfield)


Sorry, comments are closed for this post.